Cluster headaches are relatively rare compared to other types of headaches, affecting about 0.1% of the population. They are more common in men than in women, with a male-to-female ratio of about 2.5:1 to 3:1. Onset typically occurs between the ages of 20 and 40, but they can develop at any age.
In most of the cases, no testing is needed to make the diagnosis of cluster headaches. The diagnosis is based on clinical symptoms.
Cluster headaches are very painful, among the worst pain symptoms.
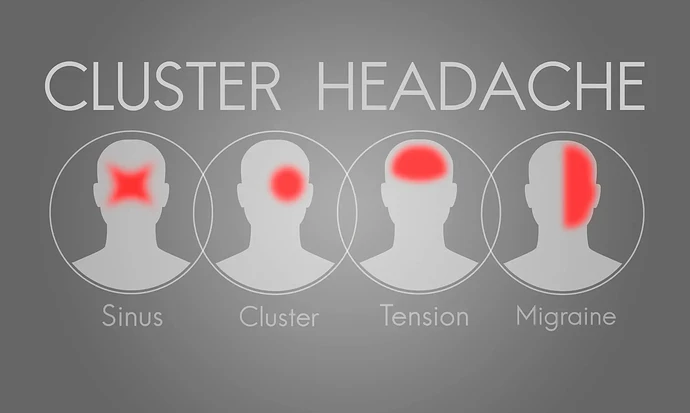
Cluster headaches are characterized by a distinct set of symptoms, including:
-
Severe, stabbing pain: Some sufferers use the terms “drilling”,or"suicid headaches" to describe the pain. Typically focused around or behind one eye, the pain can radiate to the forehead, temple, nose, and jaw. The pain is very intense and unilateral (on one side of the head).
-
Restlessness or agitation: People with cluster headaches often pace or are unable to stay still due to the pain.
-
Eye redness and tearing: The affected eye may become red and watery during an attack.
-
Nasal congestion or runny nose: This often occurs on the same side as the headache.
-
Drooping eyelid (ptosis) or swollen eyelid: The eyelid on the side of the pain may droop or swell.
-
Pupil constriction: The pupil on the affected side may become smaller.
-
Sweating on the forehead or face: Increased sweating on the side of the headache is common.
-
Attacks occur in cycles: Cluster headaches come in bouts, or clusters, lasting weeks to months, with attacks happening multiple times per day, often at the same time each day. They can be followed by remission periods without headaches.
Treatments for cluster headaches focus on both acute relief during an attack and prevention of future attacks. Here are common treatments:
Acute Treatments (for immediate relief):
-
Oxygen Therapy: Inhaling 100% oxygen through a mask at a high flow rate (12-15 liters per minute) for about 15-20 minutes is often highly effective at stopping an attack.
-
Triptans: Injectable sumatriptan (Imitrex) or nasal spray forms of sumatriptan or zolmitriptan are often used to abort cluster headaches quickly. Oral triptans are typically less effective due to the fast onset of attacks.
-
Dihydroergotamine (DHE): This is sometimes used as an injection or nasal spray for rapid relief.
-
Intranasal Lidocaine: Applying lidocaine inside the nasal passages on the affected side can sometimes abort an attack.
Preventive Treatments (to reduce the frequency and severity of attacks):
-
Verapamil: A calcium channel blocker, often used as the first-line preventive treatment for cluster headaches. Doses may be higher than typically used for other conditions, and regular monitoring (e.g., EKG) may be required.
-
Corticosteroids (Prednisone): Short-term use of oral steroids can help break a cluster cycle, but long-term use is avoided due to side effects.
-
Lithium: Commonly used to treat bipolar disorder, lithium can also be effective in preventing cluster headaches, especially in chronic cases.
-
Topiramate (Topamax): An anti-seizure medication that is sometimes used as a preventive treatment for cluster headaches.
-
Galcanezumab (Emgality): A CGRP inhibitor specifically approved for the prevention of episodic cluster headaches.
-
Nerve Blocks: Local anesthetics or steroids can be injected around the occipital nerve (back of the head) to reduce the frequency of attacks in some patients.
-
Melatonin: Some studies suggest that taking melatonin at night can help prevent cluster headaches, especially during cluster periods.
• Deep Brain Stimulation (DBS): In rare, severe cases, DBS may be used to stimulate the hypothalamus, which is thought to play a role in cluster headaches.
• Vagus Nerve Stimulation: Non-invasive vagus nerve stimulators are being studied for their potential to prevent or abort attacks.
• Psychedelic Substances: Anecdotal evidence suggests that substances like psilocybin (found in magic mushrooms) or LSD might help prevent cluster headaches, though this is still under research and not widely accepted in clinical practice.
• Avoid Triggers: Some patients find that certain triggers, such as alcohol, strong smells, or changes in sleep patterns, can precipitate an attack during cluster periods, so avoiding these triggers can help.
• Maintaining a Regular Sleep Schedule: Irregular sleep patterns can worsen cluster headache cycles, so consistent sleep habits are recommended.
Treatment plans are often individualized based on the frequency, severity, and type of cluster headaches (episodic vs. chronic).